09.07.2025
1st ASMD Workshop: Focus on Neurological and Psychiatric Involvement
Experts shared clinical and research insights into neurological and psychiatric symptoms in ASMD, ranging from infantile type A to late-onset adult cases.
Our teacher, our mentor, our doctoral advisor: Professor Michael Beck, whom we still called our "chief" with great pleasure, has gone. He leaves behind a big blank.


Experts shared clinical and research insights into neurological and psychiatric symptoms in ASMD, ranging from infantile type A to late-onset adult cases.
Clinical research for lysosomal diseases is fortunately receiving more and more attention. We would like to help you stay up to date and inform you accordingly about studies currently taking place.
An overview of the current therapy concepts with gene therapy, haematopoietic stem cell transplantation (bone marrow transplantation), enzyme replacement therapy, substrate reduction therapy and chaperone therapy is scientifically presented in the article "Precision Medicine for Lysosomal Disorders" (Jul 26 2020). Furthermore, we have tried to illustrate the topic of therapy concepts for lysosomal diseases in a comic.

Fabry Disease is an X-chromosomal inherited lysosomal storage disorder based on the deficiency of the enzyme alpha-galactosidase A. This leads to accumulation of globotriaosyl-ceramide (Gb3) in the cells of various organs. The clinical picture of M. Fabry is very heterogeneous and ranges from mild phenotypes rather in heterozygous women to severe clinical course in classically affected men. Characteristic symptoms include acroparesthesia, cardiac symptoms associated with cardiomyopathy and arrhythmias, progressive renal failure and cerebro-vascular complications (strokes). A typical eye manifestation is the cornea verticillata. Therapeutically, 3 drugs are currently available: enzyme replacement therapies with agalsidase alfa or agalsidase beta or chaperone therapy with migalastat.
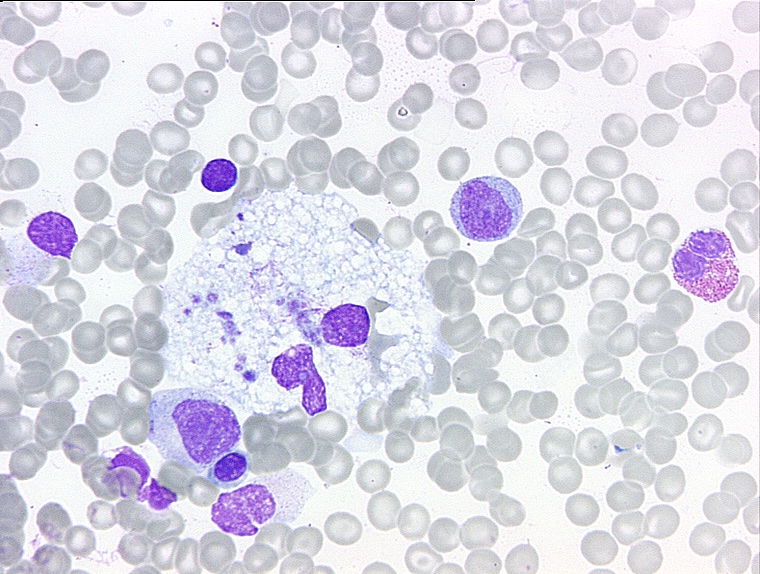
Lysosomal Storage Disorders (LSDs) are a group of more than 50 rare hereditary metabolic diseases. The diseases are characterized by an abnormal accumulation of various toxic substances in the body cells as a result of enzyme defects.
Lysosomal storage diseases affect the lysosome, a structure in the cells that breaks down substances such as proteins, carbohydrates and old cell parts so that the body can recycle them. As a result, various parts of the body may be affected, including the skeleton, brain, skin, heart and central nervous system. New lysosomal storage diseases continue to be identified.